Description
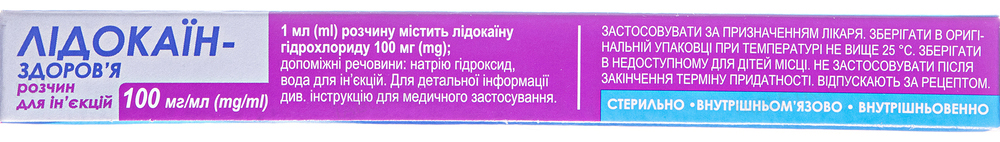
Buy Lidocaine Solution for injection 100 mg/ml 2 ml #10
Description of Lidocaine Solution for injection 100 mg/ml 2 ml:
Local anesthetic for terminal, infiltration, conduction anesthesia. The relative toxicity of lidocaine hydrochloride depends on the concentration of the solution. At low concentrations (0.5%), it does not differ significantly in toxicity from procaine, with increasing concentrations (1 and 2%), toxicity increases.
It has a local anesthetic activity due to the stabilization of the neuronal membrane, a decrease in its permeability to sodium ions, and prevents the occurrence of an action potential and the conduction of impulses.
Ingredients:
Active ingredient: lidocaine. 1 ml of solution contains lidocaine hydrochloride 100 mg;
Excipients: sodium hydroxide, water for injection.
Pharmacodynamics of Lidocaine Solution for injection 100 mg/ml 2 ml:
The antiarrhythmic activity of the drug is due to the inhibition of phase 4 (diastolic depolarization) in the Purkinje fibers, a decrease in automatism, and inhibition of ectopic foci of excitation. At the same time, lidocaine inhibits the electrical activity of depolarized, arrhythmogenic areas, but minimally affects the electrical conductivity of normal tissues. The rate of rapid depolarization (phase 0) is not affected or slightly reduced. Increases the permeability of membranes of potassium ions, accelerates the process of repolarization of cell membranes, reduces the duration of the action potential and the effective refractory period. When used in medium therapeutic doses, it practically does not change myocardial contractility, does not slow down AV conduction, and does not reduce significant blood pressure. When used as an antiarrhythmic agent for intravenous administration, the action develops after 45-90 seconds, lasts 10-20 minutes; when administered intramuscularly, the action develops after 5-15 minutes, lasts 60-90 minutes.
It has a local anesthetic activity due to the stabilization of the neuronal membrane, a decrease in its permeability to sodium ions, which prevents the occurrence of an action potential and the conduction of impulses.
Pharmacokinetics of Lidocaine Solution for injection 100 mg/ml 2 ml:
With intravenous administration, Cmax is reached after 45-90 seconds, with intramuscular injection – after 5-15 minutes. Plasma protein binding – 60-80% (depending on the dose). A stable concentration in the blood is established after 3-4 hours with continuous administration (in patients with acute myocardial infarction – after 8-10 hours). Easily passes through histohematic barriers, including the blood-brain barrier. First, it enters tissues with good blood supply (heart, lungs, brain, liver, spleen), then into adipose and muscle tissues. Penetrates through the placenta, 40-55% of the concentration of the drug used by the woman in labor is detected in the body of the newborn. Therapeutic concentration in the blood averages 0.0035 mg / ml.
It is metabolized by 90% in the liver by oxidative N-dealkylation with the formation of active metabolites: monoethylglycinexylidine and glycinexylidine, having a T½ of 2 hours and 10 hours, respectively. It has a “first pass” effect.
T½ after intravenous bolus administration is 1.5-2 hours, with prolonged intravenous infusions – up to 3 hours or more. In case of impaired liver function, T½ can increase by more than 2 times. In unchanged form, 5-20% is excreted in the urine.
Warnings and Application Features for use of Lidocaine Solution for injection 100 mg/ml 2 ml:
The introduction of lidocaine can only be carried out by medical professionals.
When treating the injection site with disinfectant solutions containing heavy metals, the risk of developing a local reaction in the form of pain and swelling increases.
During treatment, ECG monitoring is necessary. With sinus dysfunction, prolongation of the PQ interval, QRS expansion or new arrhythmia, the dose of the drug should be reduced or treatment should be stopped.
Before using lidocaine for heart disease (hypokalemia reduces the effectiveness of lidocaine), it is necessary to normalize the level of potassium in the blood.
Use with caution and in smaller doses in patients with moderate heart failure, moderate arterial hypotension, incomplete AV blockade, intraventricular conduction disorders, moderate liver and kidney function disorders (creatinine clearance of at least 10 ml/h epilepsy, after heart surgery , with a genetic predisposition to malignant hyperthermia, debilitated patients and elderly patients.
During treatment with MAO inhibitors, parenteral lidocaine should not be used.
With intramuscular administration of lidocaine, the concentration of creatinine may increase, which can lead to an error in the diagnosis of acute myocardial infarction.
This medicinal product contains less than 1 mmol (23 mg)/dose of sodium, i. e. practically free of sodium.
Use during pregnancy or lactation
During pregnancy, the drug is contraindicated. If necessary, the use of the drug breast-feeding should be discontinued.
The ability to influence the reaction rate when driving vehicles or operating other mechanisms
After the use of lidocaine, it is not recommended to engage in activities that require the speed of psychomotor reactions.
Incompatibility:
The drug should not be mixed with other drugs in the same container, except for solvents. Lidocaine precipitates when mixed with amphotericin, methohexitone, or sulfadiazine. Depending on the pH of the solution, lidocaine may not be compatible with ampicillin.
Indications for use of Lidocaine Solution for injection 100 mg/ml 2 ml:
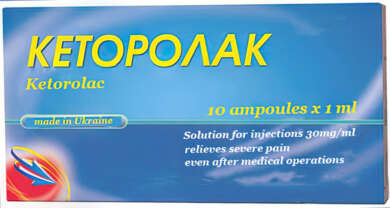
Ventricular arrhythmias (extrasystole, tachycardia, flutter, fibrillation), including during the acute period of myocardial infarction, with implantation of an artificial pacemaker, glycoside intoxication, anesthesia.
Contraindications of Lidocaine Solution for injection 100 mg/ml 2 ml:
Hypersensitivity to the components of the drug / other amide local anesthetics, a history of epileptiform convulsions to lidocaine, severe bradycardia, severe arterial hypotension, cardiogenic shock, severe forms of chronic heart failure (II-III degree syndrome-sleep), Wolff-Parkinson-White syndrome, Adams-Stokes syndrome, atrioventricular (AV) block II and III degree, hypovolemia, severe liver/kidney dysfunction, porphyria, myasthenia gravis.
Interactions:
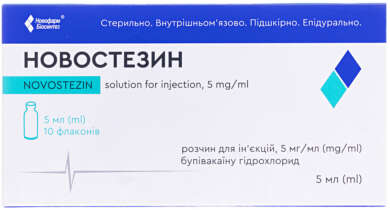
- With the combined use of lidocaine with drugs such as chlorpromazine, pethidine, bupivacaine, quinidine, disopyramide, amitriptyline, imipramine, nortriptyline, the concentration of lidocaine in the blood plasma decreases;
- Antiarrhythmic drugs (including amiodarone, verapamil, quinidine, disopyramide, aimaline) – the cardiodepressive effect is enhanced (the QT interval is prolonged and, in very rare cases, AV blockade or ventricular fibrillation may develop); simultaneous use with amiodarone can lead to the development of seizures;
- Novocaine, procainamide, procainamide – CNS excitation, delirium, hallucinations are possible;
- Curare-like drugs – muscle relaxation increases (paralysis of the respiratory muscles is possible);
- Ethanol enhances the inhibitory effect of lidocaine on respiration;
- Cimetidine reduces the hepatic clearance of lidocaine (decrease in metabolism due to inhibition of microsomal oxidation), increases its concentration and the risk of developing toxic effects;
- β-blockers slow down the metabolism of lidocaine in the liver, enhance the effects of lidocaine (including toxic ones) and increase the risk of developing bradycardia and arterial hypotension. With the simultaneous use of β-blockers and lidocaine, it is necessary to reduce the dose of the latter;
- Cardiac glycosides – the cardiotonic effect of cardiac glycosides is weakened;
- Digitalis glycosides – against the background of intoxication, lidocaine can aggravate the severity of AV blockade;
- Sleeping pills or sedative drugs – it is possible to increase the inhibitory effect on the central nervous system of hypnotics and sedative drugs;
- Narcotic analgesics (morphine, etc.) – the analgesic effect of narcotic analgesics, respiratory depression is enhanced;
- MAO inhibitors (furazolidone, procarbazine, selegiline) – the risk of arterial hypotension increases;
- Anticoagulants (including ardeparin, dalteparin, danaparoid, enoxaparin, heparin, warfarin, etc.) increase the risk of bleeding;
- Anesthesia drugs – the inhibitory effect on the respiratory center of anesthesia drugs (hexobarbital, sodium thiopental intravenously) is enhanced;
- Polymyxin B – necessary control of respiratory function;
- Rifampicin – a possible decrease in the concentration of the latter in the blood;
- Propafenone – a possible increase in the duration and severity of side effects from the central nervous system;
- Prenylamine – increases the risk of developing ventricular arrhythmias of the “pirouette” type;
- Anticonvulsants, barbiturates (phenobarbital) may accelerate the metabolism of lidocaine in the liver, lower blood concentrations, increase the cardiodepressive effect;
- Isadrin, glucagon – increases the clearance of lidocaine;
- Norepinephrine, meksiletin – the clearance of lidocaine decreases (toxicity increases); decreased hepatic blood flow;
- Acetazolamide, thiazide and loop diuretics reduce the effect of lidocaine as a result of hypokalemia;
- Midazolam – increases the concentration of lidocaine in the blood plasma;
- Drugs that cause blockade of neuromuscular transmission – the effect of these drugs is enhanced, since they reduce the conduction of nerve impulses.
Overdose of Lidocaine Solution for injection 100 mg/ml 2 ml:
May increase adverse reactions.
Symptoms: psychomotor agitation, dizziness, general weakness, decreased blood pressure, tremor, blurred vision, tonic-clonic convulsions, coma, collapse, AV blockade, asphyxia, apnea. The first symptoms of overdose in healthy volunteers occur when the concentration of lidocaine in the blood is more than 0.006 mg / kg, convulsions – at 0.01 mg / kg.
Treatment: discontinuation of the drug, oxygen therapy, anticonvulsants, vasoconstrictors (norepinephrine, mezaton), anticholinergics. The patient should be in a horizontal position; it is necessary to provide access to fresh air, oxygen supply and / or artificial respiration. CNS symptoms are corrected with short-acting benzodiazepines/barbiturates. If an overdose occurs during anesthesia, a short-term muscle relaxant should be used. To correct bradycardia and conduction disturbances, atropine (0.5-1 mg intravenously) is used, with arterial hypotension – sympathomimetics in combination with β-adrenergic receptor agonists. In case of cardiac arrest, immediate resuscitation is indicated. It is possible to carry out intubation, artificial ventilation of the lungs. In the acute phase of overdose, dialysis is ineffective.
Side effects:
- From the nervous system: CNS excitation (when used in high doses), anxiety, headaches, dizziness, sleep disturbance, confusion, drowsiness, loss of consciousness, coma, sensory disturbance, motor block; in patients with hypersensitivity – euphoria, tremor, trismus, restlessness, paresthesia, convulsions;
- On the part of the organs of vision: nystagmus, reversible blindness, diplopia, flashing “flies” before the eyes, photophobia, conjunctivitis;
- On the part of the hearing organs: hearing impairment, tinnitus, hyperacusis;
- From the side of the cardiovascular system: when used in high doses – arrhythmia, bradycardia, slowing of cardiac conduction, transverse heart block, cardiac arrest, peripheral vasodilation, collapse; very rarely – tachycardia, increase / decrease in blood pressure, pain in the heart;
- From the digestive system: nausea, vomiting;
- From the respiratory system: shortness of breath, rhinitis, depression or respiratory arrest;
- Allergic reactions: extremely rarely – skin rash, urticaria, itching, generalized exfoliative dermatitis, angioedema, anaphylactic reactions (including anaphylactic shock);
- Others: sensation of heat, cold or numbness of the extremities, swelling, weakness, malignant hyperthermia;
- Local reactions: a slight burning sensation that disappears with an increase in the anesthetic effect (within 1 minute), hyperemia.
Storage:
Store below 25°C in original packaging. Keep out of the reach of children.
Shelf life:
3 years.




Reviews
There are no reviews yet.